
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
282
AFRICA
sternum retraction and electric cautery injury.
1-3
Other causes of
pseudoaneurysm of the ITA are idiopathic, trauma, penetrating
injury, infection, PMI and central vein cannulation.
1,4,5
Massive bleeding may result in life-threatening conditions.
Pseudoaneurysm of the ITA is commonly diagnosed using
medical imaging modalities such as CT and ultrasonography;
however, it could also be diagnosed through surgical exploration.
1
In our case, ITA aneurysm occurred in the delayed phase after
surgery and the pathogenesis of the right ITA pseudoaneurysm
formation was uncertain. Direct injury during the opening
or closure of the sternum or a manoeuvre during PMI was
suspected as the cause of the ITA pseudoaneurysm, although
it was unlikely that it was caused by PMI because this was
performed using a cut-down technique. The fragility of vessels
in patients with Marfan syndrome was also considered to
contribute to the formation of the ITA pseudoaneurysm.
CT is a useful diagnostic tool; however, detecting the origin
of bleeding using this modality is difficult. Selective angiography
allowed precise identification of the origin of bleeding. Nanami
et al
. reported that ITA angiography was a useful diagnostic
tool for the treatment of ITA pseudoaneurysm.
1
Furthermore,
the bleeding could be controlled soon after the diagnosis by
simultaneous embolisation of the ITA.
Conclusion
Although the possibility of the occurrence of a delayed
pseudoaneurysm or bleeding of the ITA is low after a median
sternotomy procedure, postoperative management of patients
who have undergone median sternotomy should also focus on
the prevention or early detection of pseudoaneurysm of the ITA
to avoid life-threatening conditions.
References
1.
Namai A, Sakurai M, Akiyama M. Poststernotomy pseudoaneurysm
of the internal mammary artery
. Gen Thorac Cardiovasc Surg
2008;
56
:
344–346.
2.
Ayaon Albarrán A, Blázquez González JA, Hernández Cabrero T,
González Villegas E. Internal mammary artery pseudoaneurysm follow-
ing a robicsek sternal closure.
J Card Surg
2017;
32
: 264–265.
3.
Falconieri F, Raevsky E, Davies S, Moat N. Pseudoaneurysm of a branch
of left internal mammary artery: a late and potentially fatal complication
after redo-sternotomy.
Interact Cardiovasc Thorac Surg
2015;
20
: 866–867.
4.
Kang K, Maholic R, Kang G. Successful coil embolization of a bleeding
internal thoracic artery that caused severe hypotension immediately after
permanent pacemaker placement.
Indian Heart J
2015;
67
: 493–494.
5.
San Norberto EM, Cilleruelo A, Martin-Pedrosa M, Taylor J, Garcia-
Yuste M, Vaquero C. Endovascular treatment of posttraumatic pseudoa-
neurysm of the internal mammary artery.
Ann Vasc Surg
2014;
28
: 743.
e1–743.e5.
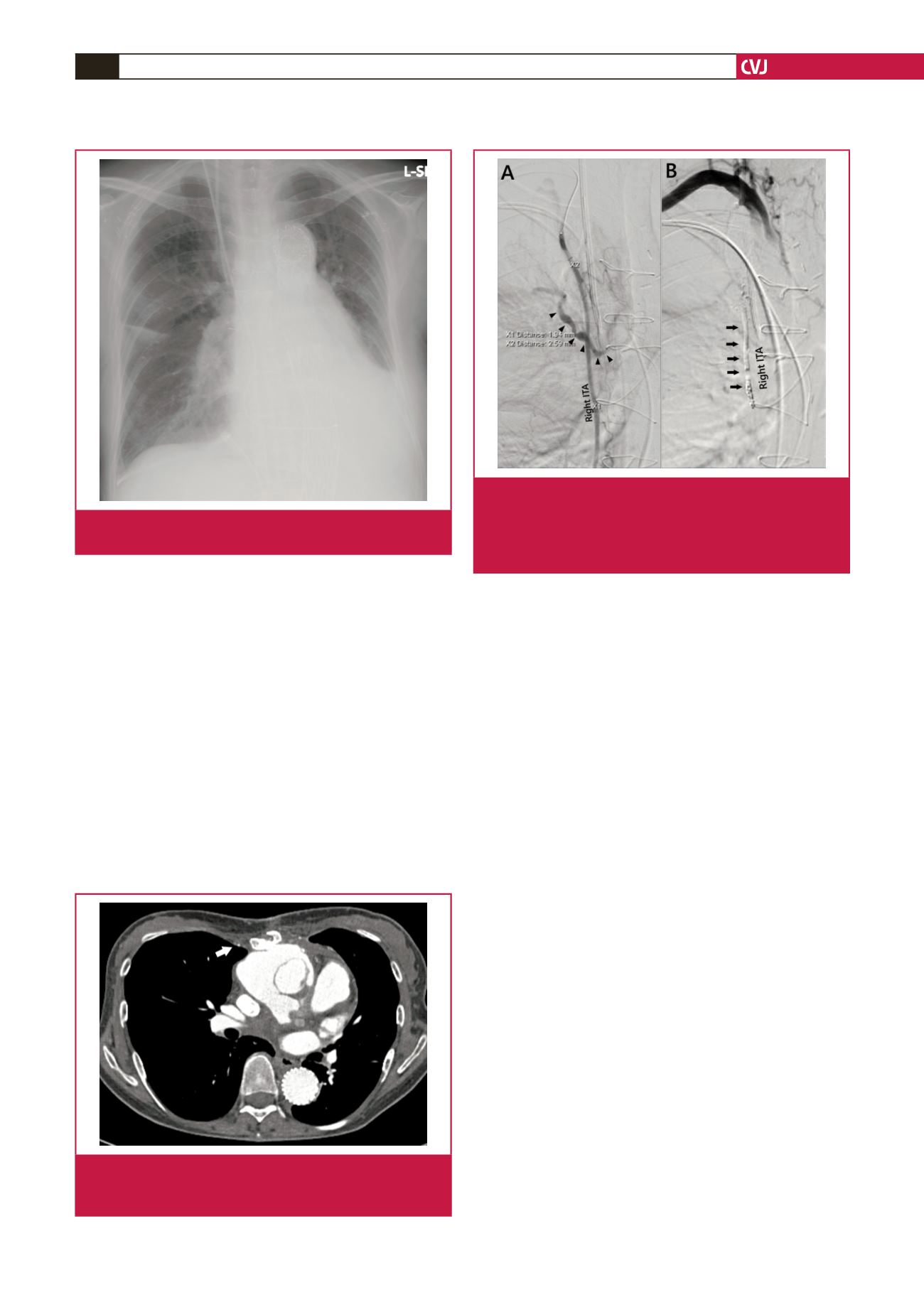
Fig. 2.
Chest radiography performed the day before pacemak-
er implantation reveals minimal right pleural effusion.
Fig. 3.
Computed tomography before redo aortic root surgery
reveals a normal internal thoracic artery and its branch
vessels.
Fig. 4.
A: Selective angiography of the right internal thoracic
artery reveals that the bleeding originated from a
branch of the right internal thoracic artery (arrowhead).
B: The right internal thoracic artery was selectively
embolised (arrow) and bleeding was controlled.



















