
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 4, July/August 2021
202
AFRICA
attitudes and practice towards hypertension and TLC, and the
barriers patients perceived to implementing these changes.
The lifestyle changes participants were questioned on were
salt reduction, weight loss, regular exercise, smoking cessation
and moderation of alcohol intake. Overall, the results of the
study showed that hypertensive subjects possessed a good
general knowledge regarding TLC and were implementing these
modifications to a certain extent.
The lifestyle change found to be most implemented was
abstaining from alcohol; none of the respondents reported
any alcohol intake, which is most probably due to the cultural
and religious beliefs of the area. This was followed by smoking
cessation (96.4%), where cultural background probably played
a big role. Most respondents were never smokers in their early
years. A high percentage of respondents (84.8%) were actively
reducing their salt intake since diagnosis with hypertension,
which can only be explained by the fact that patients were
actively adopting healthier lifestyles. Exercise was the lifestyle
modification least adhered to by hypertensive patients, where
60% admitted to not regularly exercising.
The reason reported most often by participants for not
implementing each of the lifestyle modifications was ‘not
thinking it matters’ or ‘laziness’, which could be interpreted
as patients not being adequately motivated by health givers to
adopt healthier lifestyles and not being educated properly on
their importance as adjuncts to pharmacological therapy.
Participants were most knowledgeable on the importance of
reducing salt intake in managing hypertension (93.8%), which
was reflected in their implementation, as it was the lifestyle
change most applied that could not be explained by the cultural
background of the study area. More than half of the respondents
answered incorrectly to whether alcohol consumption affected
blood pressure, suggesting the idea that abstaining from alcohol
consumption was more of a cultural issue.
A high percentage of participants (71.4%) answered correctly
that regular exercise can help lower blood pressure but it was not
reflected in their implementation, exercise being the modification
least applied. This implies that other than just being given
the knowledge of such lifestyle changes, patients need to be
motivated adequately by doctors. Further affirming this view is
the fact that no association was found between patients’ level of
knowledge and their degree of implementation of TLC.
Although duration of consultation was found to be associated
with participants’ level of knowledge (
p
= 0.039), it did not affect
their degree of implementation, which may imply that different
methods and skills of motivating patients to adhere to lifestyle
changes may be needed and not simply spending more time on
each consultation.
Perhaps worryingly, no association was found between
previous cardiovascular events and patients’ knowledge level, as
a previous event would usually stipulate more intense counselling
of lifestyle changes. This requires further study, assessing
clinicians’ practice in this regard.
Upon reviewing the literature in comparison with the results
of this study, the general level of knowledge of participants
was found to be comparable to most studies on this topic, one
such study conducted on attitudes and practice in Cape Coast
in Ghana,
7
another one being conducted in South Africa.
8
Salt
restriction was the most well-known lifestyle change in both,
with both populations having good knowledge on hypertension
management.
Results from a Canadian national survey in terms of
implementation also partially agreed with the results of this study,
with the population having a generally high implementation
level.
9
Salt restriction was the lifestyle change most frequently
adhered to. It was also comparable with this study with regard
to perceived barriers to implementation, as ‘not wanting to do
so’ and ‘not feeling it matters’ were both frequently reported
barriers, similar to that reported in this study. This further
confirms the idea that patients were not being adequately
motivated by health givers.
Of the studies conducted on awareness of patients of
hypertension and its associated risk factors, one such study
carried out in Khartoum found uncontrolled hypertension to be
associated with a lack of awareness towards lifestyle changes and
adherence to medication. As far as the researcher’s knowledge
is concerned, no other study has been undertaken assessing
the knowledge, attitude and practice of hypertensive patients
towards TLC specifically.
One of the aspects of this study was to examine whether
patients were receiving counselling on lifestyle changes from
their doctors and how long they perceived the consultation took.
About 85% of participants reported receiving advice on lifestyle
change. This proportion is surprisingly high when compared to
results reported by a study from Australia,
10
where less than 30%
of patients recalled ever receiving advice on lifestyle change.
This discrepancy might be explained by the difference in study
population as our study recruited from speciality cardiology
clinics as opposed to primary practice. The same can be
assumed for the generally high level of knowledge and degree of
implementation demonstrated by participants in this study.
Limitations
The fact that subjects were selected from referral clinics could
be considered a limitation of this study. Other limitations are
the small sample size of 112 participants, and that the hospitals
selected were from Khartoum and Bahri localities only. Hence
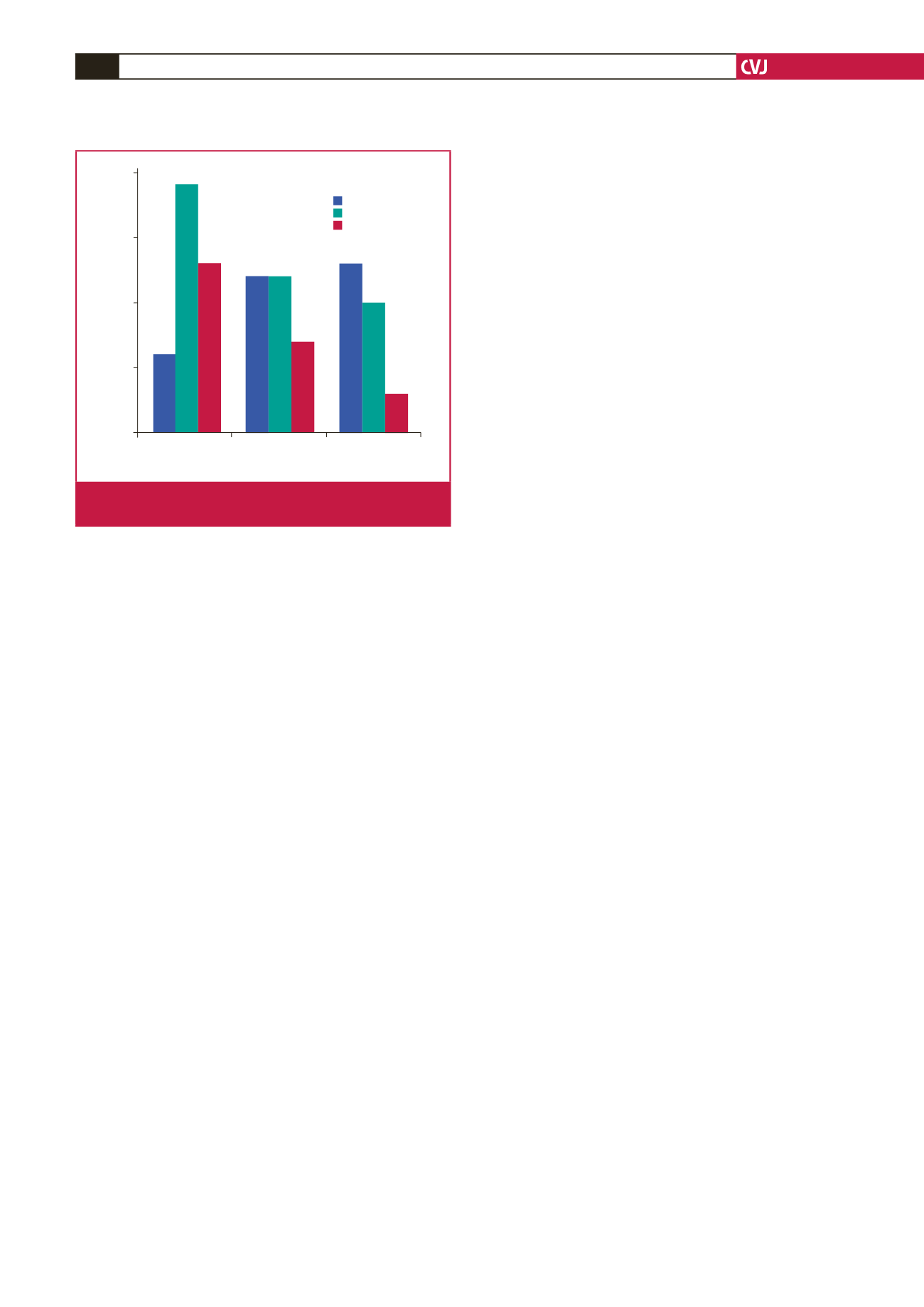
Count
0
5
10
15
20
Consulation time
< 5 min
5–10 min
> 10 min
Knowledge level
above average
average
below average
Fig. 8.
Association between consultation time and knowledge
level.



















