CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
AFRICA
213
All variables showing an association (
p
≤
0.05) with
pneumonia post cardiac surgery were then entered into a
forward stepwise multivariate logistic regression model. A
two-sided
p-
value
<
0.05 was considered significant in the
multivariate logistic regression model. Adjusted odds ratios
(AORs), 95% confidence intervals (CIs), and two-tailed
p-
values
were calculated for all variables retained in the multivariate
logistic regression model. Statistical analyses were carried out
using the statistical packages for SPSS 15.0 for Windows (SPSS
Inc., Chicago, IL, USA).
Results
The study group comprised 162 patients who underwent cardiac
surgery. The mean age of the patients was 65.57
±
10.48 years
(range 43–84 years), and 83 (51%) were male. Of 162 operations,
140 were coronary artery bypass graft (CABG) surgery, and 22
patients underwent valve replacement surgery. Sixteen CABG
operations were performed without cardiopulmonary bypass
(CPB).
Before surgery, 20 patients were in New York Heart
Association (NYHA) functional class I, 101 patients were
in class II, and 41 were in class III. Pre-operative co-morbid
diseases were diabetes in 106 patients, hypertension in 111
patients, chronic obstructive pulmonary disease (COPD) in 43
patients, peripheral artery disease in 10 patients and AF in 29
patients. Ninety-one (56.2%) patients were tobacco users. The
patients’ characteristics and peri-operative variables are shown
in Table 1.
Postoperative pneumonia was detected in 21 (13%) patients.
Mean remaining time in the intensive care unit and mean length
of hospitalisation were longer for patients with postoperative
pneumonia compared to the patients without postoperative
pneumonia (4.5
±
2.7 vs 3.1
±
1.1 days,
p
<
0.001; 13.1
±
9.4
vs 8.8
±
4.3 days,
p
=
0.001). There was no difference between
CABG and valve-replacement surgery regarding postoperative
development of pneumonia (
p
=
0.435).
Pre-operative heart rate was related to postoperative incidence
of pneumonia (
p
=
0.047). The percentage of patients with
previous COPD and diabetes was greater in the group with
postoperative pneumonia. The remaining patients’ characteristics
regarding pre-operative variables were similar between the
groups.
Whereas none of the intra-operative variables had any effect
on development of pneumonia, many postoperative variables
were significant risk factors. In patients with postoperative
pneumonia, intubation time was longer, postoperative urea,
creatinine and potassium levels were higher, more chest tube
drainage was encountered, and the need for transfusion of pRBC
and FFP was increased.
All variables showing an association (
p
≤
0.05) with
occurrence of postoperative pneumonia were then entered into
a forward stepwise multivariate logistic regression model. The
following variables were included in the multivariate model:
pre-operative heart rate, previous diabetes, previous COPD,
postoperative urea, creatinine and potassium levels, extubation
time, number of transfused FFP units, number of transfused
pRBC units and postoperative AF. Upon logistic regression
analysis of these risk factors, pRBC transfusion, previous COPD
and postoperative AF remained as independent predictors for the
development of pneumonia post cardiac surgery (Table 2).
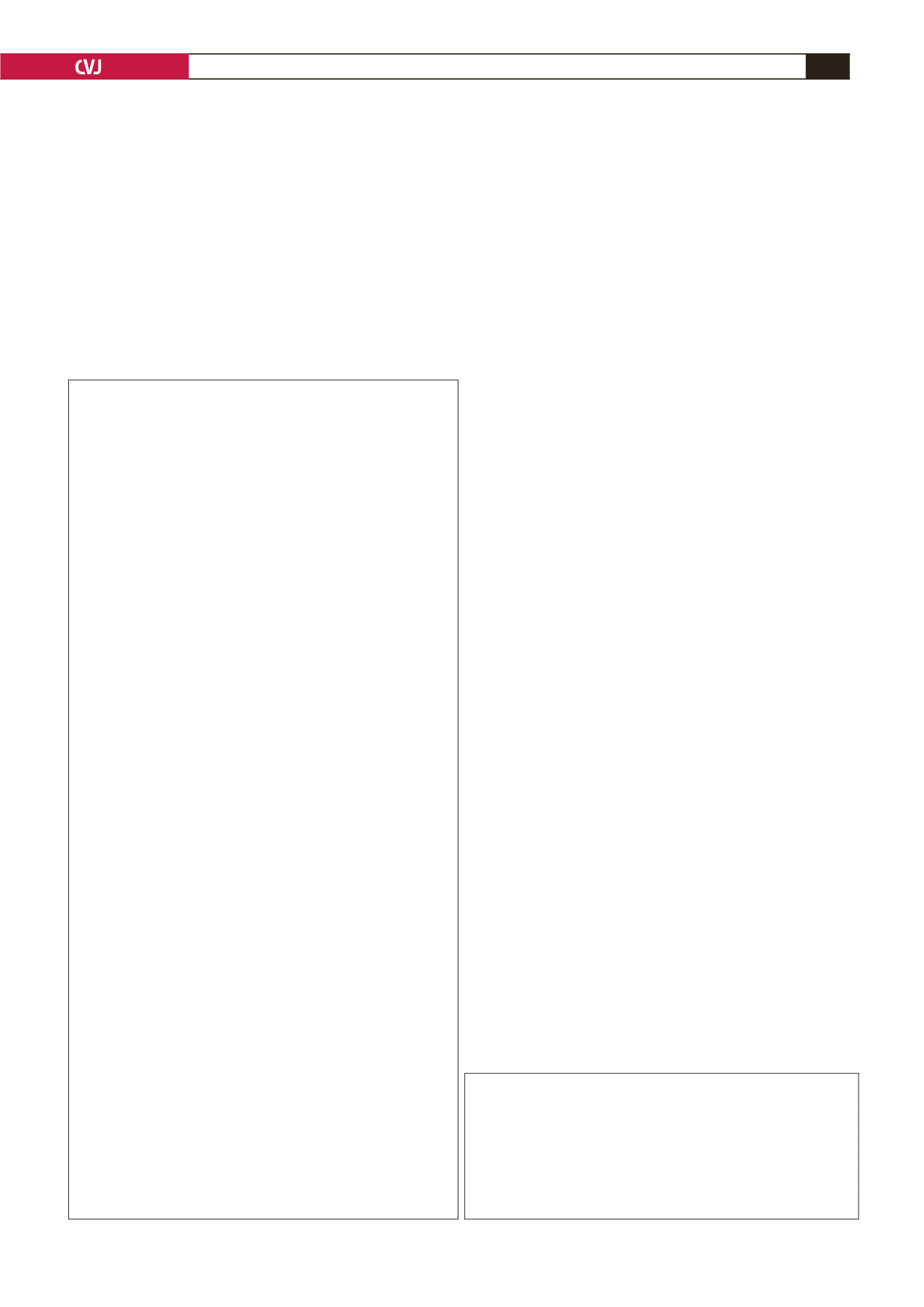
TABLE 1. EFFECT OF PATIENTS’ CHARACTERISTICS
AND PERI-OPERATIVEVARIABLES ON DEVELOPMENT OF
PNEUMONIA POST CARDIAC SURGERY
Patients
without
pneumonia
(
n
=
141)
Patients with
pneumonia
(
n
=
21)
p
-value
Male,
n
(%)
72 (51.1)
11 (52.4)
0.911**
Age (years)
65.3
±
10.4 67.5
±
11.0 0.362*
Pre-operative variables
NYHA class,
n
(%)
0.889**
I
17 (12.1)
3 (14.3)
II
89 (63.1)
12 (57.1)
III
35 (24.8)
6 (28.6)
Ejection fraction (%)
50.5
±
8.7 47.6
±
9.4 0.170*
Heart rate (/min)
92.2
±
6.3 89.2
±
7.4 0.047*
Mean blood pressure (mmHg)
91.7
±
9.7 88.3
±
6.9 0.130*
Body surface area (m
2
)
1.7
±
0.1 1.7
±
0.2 0.242*
Urea (mg/dl)
40.2
±
14.3 44.7
±
13.1 0.174*
Creatinin (mg/dl)
1.0
±
0.2 1.0
±
0.2 0.403*
Potassium (mmol/l)
4.3
±
0.4 4.2
±
0.5 0.855*
Hypertension,
n
(%)
97 (68.8)
14 (66.7)
0.845**
Hyperlipidaemia,
n
(%)
89 (63.1)
14 (66.7)
0.753**
Tobacco usage,
n
(%)
79 (56)
12 (57.1)
0.924**
Peripheral arterial disease,
n
(%)
9 (6.4)
1 (4.8)
0.774**
Atrial fibrillation,
n
(%)
25 (17.7)
4 (19)
0.884**
COPD,
n
(%)
27 (19.1)
16 (76.2)
<
0.001**
Diabetes mellitus,
n
(%)
88 (62.4)
18 (85.7)
0.037**
Intra-operative variables
Off pumpn,
n
(%)
13 (9.2)
3 (14.3)
0.469**
Cross-clamp time (min)
36.2
±
10.8 37.8
±
9.8 0.552*
CPB time (min)
60.4
±
16.9 61.2
±
15.0 0.859*
Total operation time (min)
114.9
±
20.3 114.8
±
15.0 0.971*
Need for inotropic support,
n
(%) 30 (21.3)
8 (38.1)
0.091**
Postoperative variables
Extubation time (hour)
7.5
±
2.8 25.0
±
21.3
<
0.001*
Chest tube drainage (ml)
610.6
±
286.0
733.3
±
287.4
0.069*
Units of transfused FFP
2.9
±
1.5 4.8
±
3.3
<
0.001*
Units of transfused pRBC
5.8
±
1.6 10.8
±
3.3
<
0.001*
Urea (mg/dl)
45.2
±
15.7 57.8
±
21.6 0.001*
Creatinine (mg/dl)
1.1
±
0.4
1.3
±
.5
0.009*
Potassium (mmol/l)
3.7
±
0.7 4.1
±
1.0 0.008*
Atrial fibrillation,
n
(%)
25 (17.7)
13 (61.9)
<
0.001**
*Student’s
t
-test, **Fisher’s exact test.
COPD: chronic pulmonary obstructive disease, CPB: cardiopulmonary
bypass, FFP: fresh frozen plasma, pRBC: packed red blood cells.
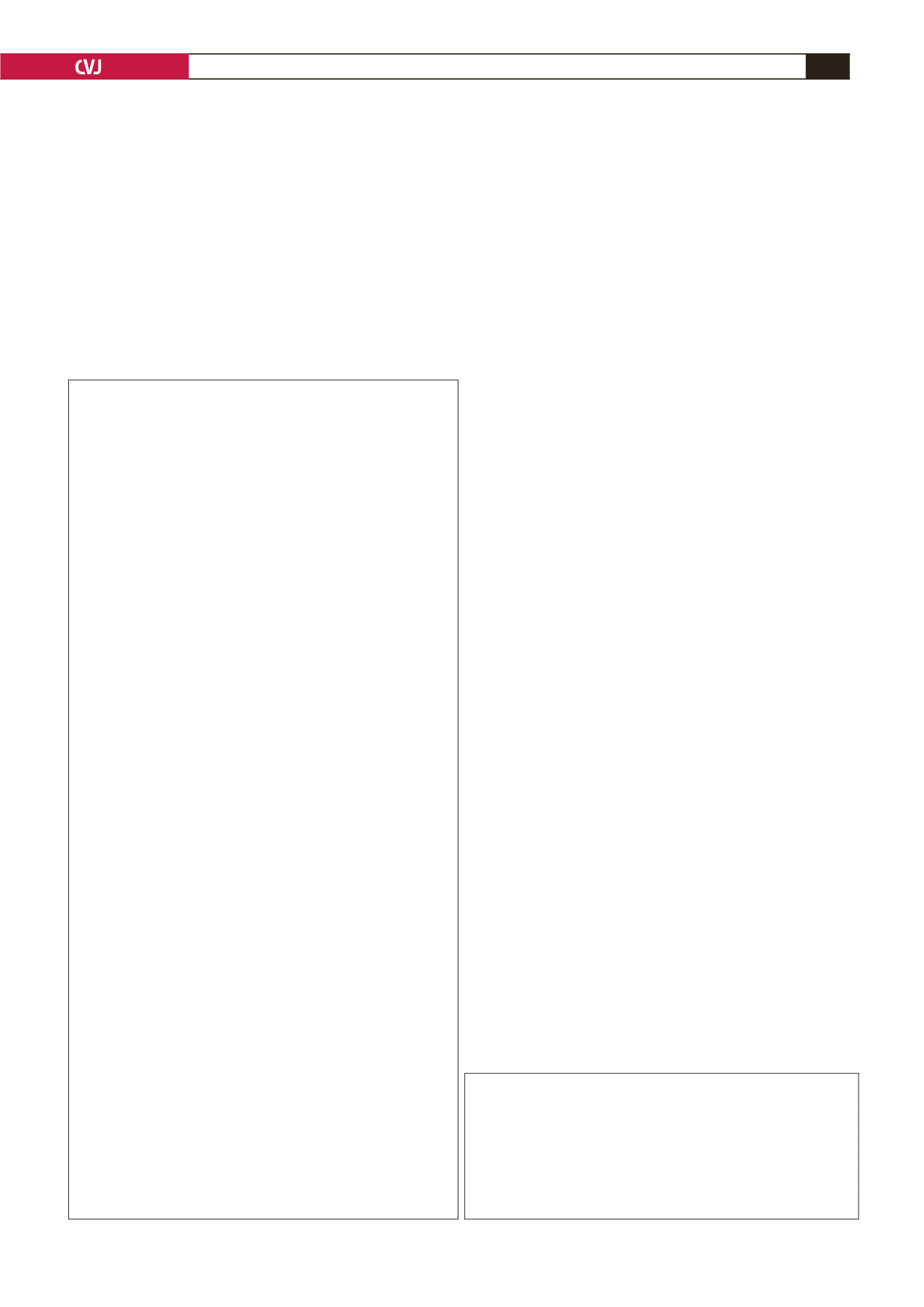
TABLE 2. THE OUTCOMES OF FORWARD STEPWISE BINARY
LOGISTIC REGRESSIONAND ODDS RATIO
Variables
β
SE Wald
OR (95% CI)
p
-value
pRBC transfusion 0.910 0.220 17.131 2.484 (1.614–3.821)
<
0.001
Previous COPD 3.026 0.932 10.530 20.613 (3.315–128.191) 0.001
Postoperative AF 1.732 0.855 4.100 5.653 (1.057–30.228)
0.043
pRBC: packed red blood cells, COPD: chronic obstructive pulmonary
disease, AF: atrial fibrillation.