
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 2, March/April 2018
AFRICA
99
more frequent INR monitoring and contraceptive counsel-
ling.
Conclusions:
Our study demonstrates that participation in
clinical research on RHD can have a positive impact on
patient management. Furthermore, REMEDY has led to
increased patient awareness and improved healthcare workers’
knowledge and efficiency in caring for RHD patients.
Keywords:
rheumatic heart disease, REMEDY study, clinical
research, low- and middle-income countries, implementation
Submitted 30/7/17, accepted 19/11/17
Published online 19/3/18
Cardiovasc J Afr
2018;
29
: 98–105
www.cvja.co.zaDOI: 10.5830/CVJA-2017-054
Rheumatic heart disease (RHD) is the principal cause of
valvular heart disease-related mortality and morbidity in low-
and middle-income countries (LMICs). It predominantly affects
children and young adults and is potentially responsible for
approximately 233 000 deaths per year worldwide.
1
However,
contemporary data documenting the presentation, clinical
course, complications, and ‘real-world’ treatment of RHD are
relatively scarce.
The Global Rheumatic Heart Disease Registry (REMEDY)
was a prospective registry of 3 343 patients with RHD from 25 sites
in 14 LMICs that was conducted from January 2010 to November
2012.
2
It documented both clinical and echocardiographic
characteristics of the patients, and outcomes and current treatment
practices, with particular reference to adherence to secondary
prophylaxis with penicillin and oral anticoagulation regimens.
3,4
The outcomes of REMEDY have drawn attention to a number
of concerns. First, although patients were young, two-year case
fatality rate was high.
4
Second, post-primary school education
level is associated with lower risk of death, and third, patients
from low- and lower-middle-income countries have higher age-
and gender-adjusted mortality rates than patients from upper-
middle-income countries. Fourth, valve surgery is more frequently
undertaken in upper-middle-income countries than in low- and
lower-middle-income countries. These findings have motivated
further research and changes in clinical practice relating to RHD
at many of the original REMEDY investigation sites.
5-8
It is well known that clinical outcomes of patients who
participate in clinical research are superior to those in real-
world practice.
9
In randomised trials, this effect may relate to
selective enrolment but the explanations in registry studies are
poorly defined. Therefore, our study aimed to identify the major
challenges and opportunities encountered by investigators and
members of the research teams during the study and to provide
a useful reference for researchers working on future similar
projects in LMICs.
Methods
We created an online survey comprising four sections, with a
total of 45 questions (Table 1). The online survey addressed
questions concerning patient follow up, administration and
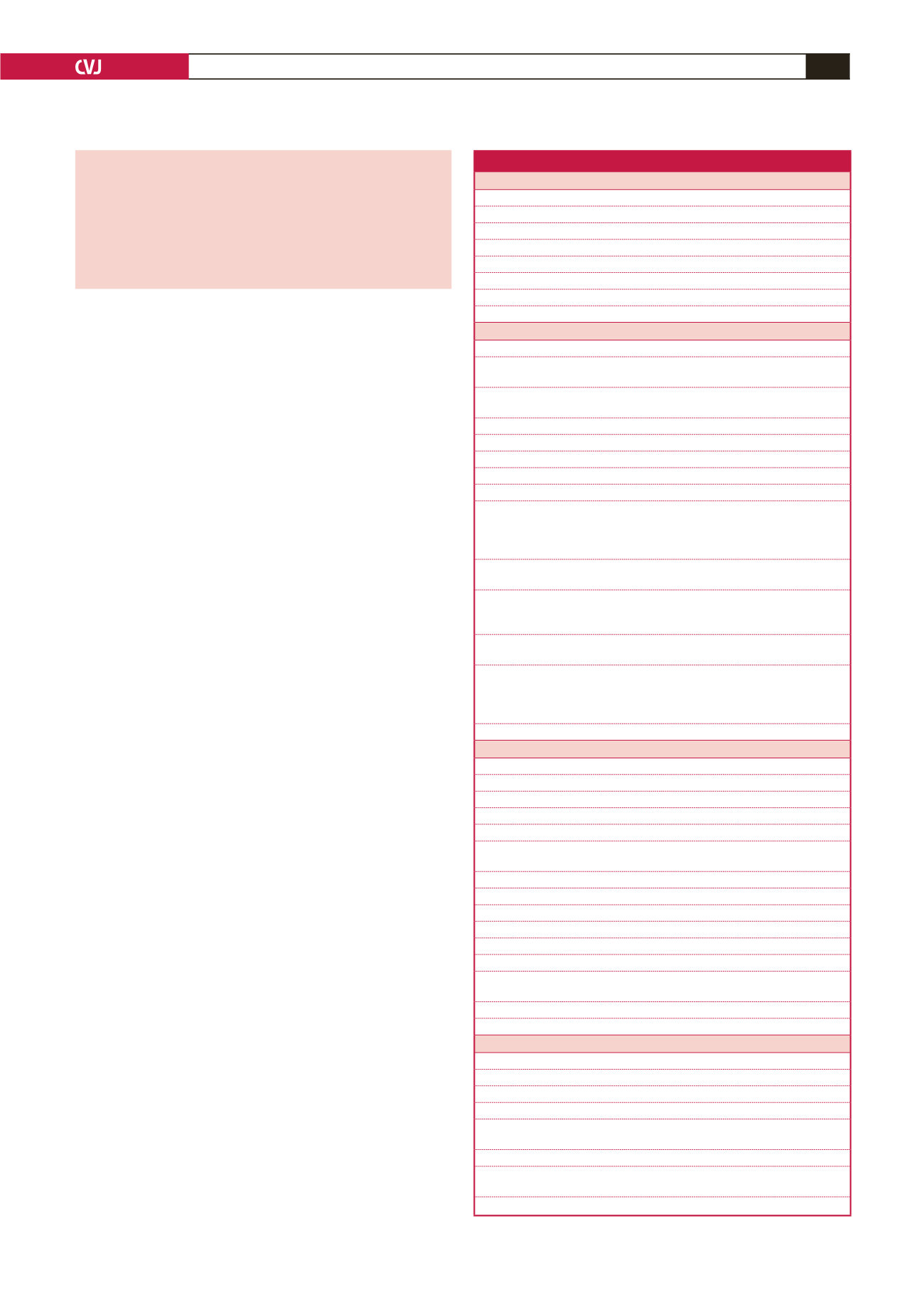
Table 1. Challenges and opportunities: the REMEDY study (online survey)
Section 1: Personal details
1. Name
2. Role
3. Site/centre number
4. Name of hospital/facility
5. Country
6. Would you be interested in participating in the telephone interview?
7. If yes, how would you prefer to be contacted?
8. Please specify your contact details and best time/day for calling
Section 2: About your site
9. How would you describe your site?
10. Before REMEDY, had your site ever conducted a local/single-site research study
before?
11. Before REMEDY, had your site ever conducted a multi-centre research study
before?
12. How many members of staff on your site participated in REMEDY?
13. Was a GCP course offered on-site?
14. If yes, how many members of staff completed a GCP course?
15. If no, did any of your staff complete GCP training as part of REMEDY?
16. Did you attend a REMEDY investigator meeting?
17. If yes, how far do you agree with the following statement?
‘The investigator meeting was productive and supportive, providing an opportunity
for learning and clarification. Adequate time was provided to give and receive feed-
back. I felt confident to continue with the conduct of the study after the meeting.’
18. Did you have a site initiation visit from a representative from the UCT project
coordination office?
19. If yes, how useful did you find it?
‘I felt I was given complete information and adequate time to learn and ask
questions. I was confident to conduct the study at the end of the visit.’
20. Did you have an on-site monitoring visit from a representative from the UCT
project coordination office?
21. If yes, how useful did you find it?
‘The visit was productive and supportive, providing an opportunity for learning
and clarification. Adequate time was provided to give and receive feedback. I felt
confident to continue with the conduct of the study after the visit.’
22. What would you change about the training you received?
Section 3: Organisation and accessibility
23. Was INR available on-site?
24. If yes, on-site INR results were generally available
25. Results were made available by
26. If not available on-site, where was testing performed?
27. If not available on-site, how long did it take to receive results?
28. What supplies/equipment did you purchase specifically for conducting the
REMEDY study?
29. What type of echo equipment did you use?
30. Did you have easy access to an ECG machine?
31. Did you have access to ECG paper?
32. CRFs were sent to the UCT project coordination office
33. During the study, my access to REMEDY email and internet was
34. During the study, medical records at my site were
35. Did you change the way you manage your RHD patients as a result of participating
in the REMEDY study?
36. Please check any administrative changes due to the REMEDY study
37. Please check any clinical changes due to the REMEDY study
Section 4: Patients
38. Where were baseline ECGs conducted?
39. Where were baseline echos conducted?
40. Did your site experience stock-out problems for penicillin during the study?
41. Did your site experience stock-out problems for anticoagulants during the study?
42. Did your site experience stock-out problems for other cardiac drugs during the
study?
43. What were the most difficult challenges you faced upon following up patients?
44. Did you experience any other challenges not mentioned above upon following up
patients?
45. How did you resolve them?

















