
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 2, March/April 2018
AFRICA
101
Strategies to reduce losses to follow up included initiation of
home visits to patients who had missed appointments, collection
of several telephone numbers from patients and relatives,
initiation of telephone reminders before clinics, sketching patient
residences on a map in the absence of a formal address system
and educating patients about the importance of regular follow
up.
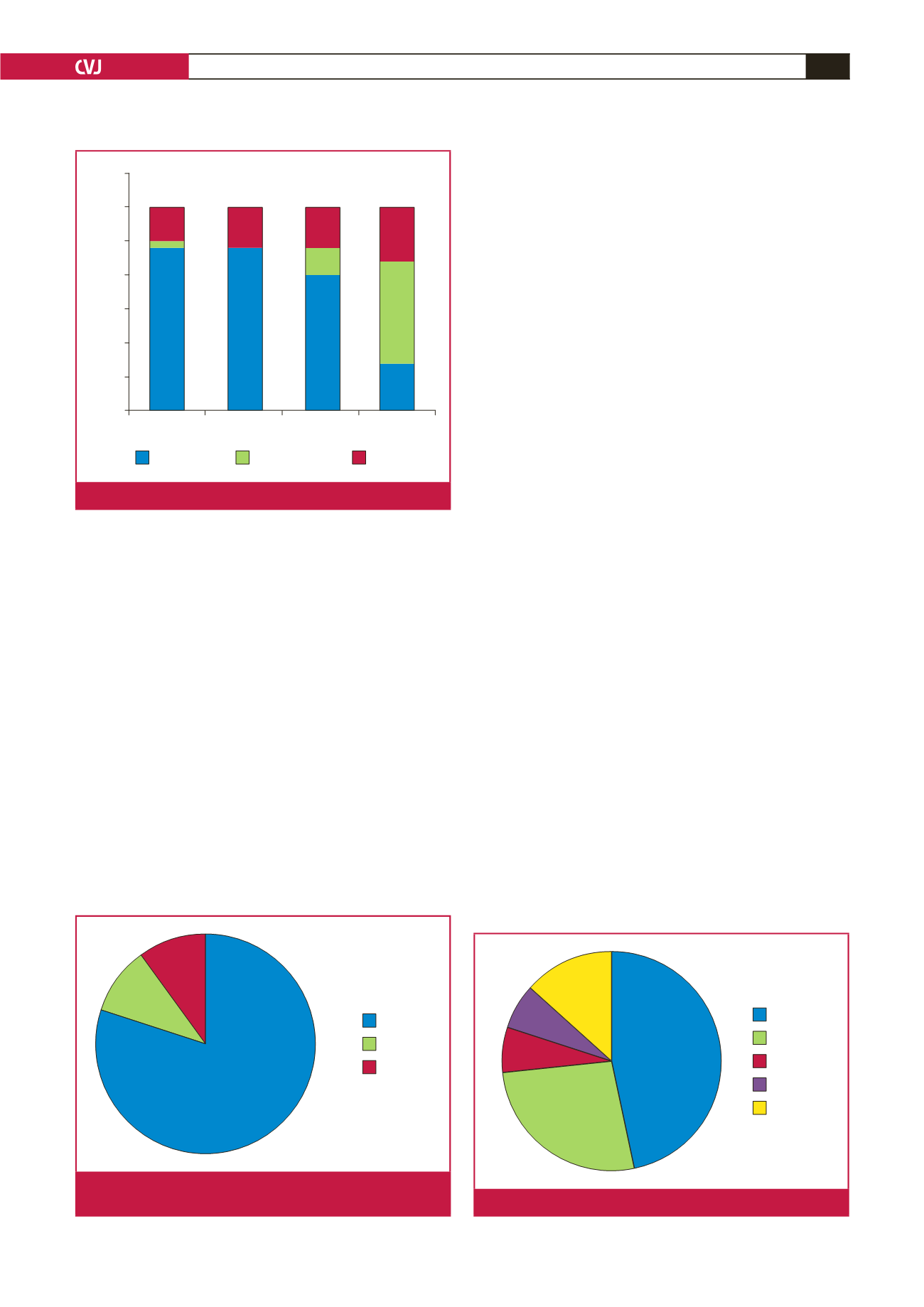
Administration and clinical management: the majority of
responses (24/30) were positive when asked whether participation
in REMEDY changed their management of RHD patients (Fig.
4). Administrative changes included increased frequency of
follow-up appointments (14/24), increased information noted
in patient records (13/24), and changes to clinic times and
booking systems (6/24). Clinical changes included more rigorous
prescribing practices for penicillin prophylaxis (15/24) and
warfarin (6/24), more frequent international normalised ratio
(INR) monitoring (11/24), and increased efforts to provide
contraceptive counselling to post-menarchal females (9/24).
Staff training: in total, 8/30 respondents’ sites offered a good
clinical practice (GCP) course on-site that was completed by the
majority of staff at 5/8 sites. On-siteGCP training was unavailable
to 18/30 respondents. Nevertheless, 10/18 respondents stated that
staff completed GCP courses via other mechanisms, such as
online courses.
Twenty-four/30 respondents attendedaREMEDYinvestigator
meeting; 21/24 agreed that the meeting was productive and
supportive, that adequate time was provided to give and receive
feedback and that they felt confident to continue with the study
after the meeting. Ten/30 respondents received a site initiation
visit from a representative of the project coordination office
(PCO); 10/10 agreed that they were given adequate information
and time to learn during the visit and that they felt confident to
conduct the study afterwards. Thirteen/30 received an on-site
monitoring visit from a representative of the PCO. Of these,
12/13 agreed that the visit was productive and supportive,
provided opportunity for learning, clarification and feedback,
and increased their confidence to continue with the study.
When asked whether they would change anything about
the training they received, most (19/30) respondents did not
answer, 3/30 stated that they would not change anything and
8/30 made suggestions for future related studies that included
clarification about specific medical terminology, drug categories
and diagnostic tests, increased numbers of investigator meetings
and monitoring visits, mandatory GCP courses and increased
online communication.
On-site resources: most (26/30) respondents’ sites had
participated in single-site research before REMEDY. Most
(20/26) had also participated in multi-centre research. As a result,
different sites had different capacities to conduct research over
two years. For example, numbers of staff greatly varied across
REMEDY sites. Fourteen/30 respondents’ teams comprised one
to five individuals, 8/30 comprised five to 10 individuals, 2/30
comprised 10 to 15 individuals, and 2/30 had over 15 members
of staff dedicated to the project (Fig. 5).
INR monitoring was available on 23/30 respondents’ sites.
On-site INR results were available at point of care (5/23), on
the same day as patient visits (9/23), after visits (6/23) or at
times not specified on the survey, such as the day before visits
(3/23). Results were made available by telephone (4/23), hard-
copy printouts (16/23) or electronic devices (1/23). INR was not
available on-site for 7/30 respondents and instead was performed
at nearby hospitals, private laboratories or non-governmental
organisation-run clinics. Off-site results were received on the
80%
10%
10%
Impact
No answer
No impact
Fig. 4.
Online survey: impact of REMEDY on patient manage-
ment.
1 to 5
10 to 15
No answer
5 to 10
Over 15
14
8
2
2
4
Fig. 5.
Online survey: numbers of on-site REMEDY staff.
Challenging
Not challenging
Not answered
Invalid telephone
numbers
Long
distances
Medical costs
to patients
Language
barriers
35
30
25
20
15
10
5
0
24
24
20
4
5
6
6
8
15
7
1
Respondents
Fig. 3.
Common barriers to follow up.

















