
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 2, March/April 2020
100
AFRICA
to explain these relations. Furthermore, insulin resistance may be
a consequence of CKD rather than a cause,
30
and reductions in
eGFR may result in a reduced clearance of circulating substances
and increases in circulating resistin concentrations. However,
being a community-based study, few participants had late stages
of CKD, which is more likely to result in insulin resistance or a
reduced clearance of circulating resistin. Indeed, the relationships
between insulin resistance or resistin concentrations and eGFR
were largely in the early CKD stage range.
Second, the appropriate formula for calculating eGFR from
serum creatinine concentrations in groups of black African
ancestry is uncertain and ethnic-specific formulae have not been
identified in Africa. As the relationships noted were largely
in those with an eGFR > 60 ml/min/1.73 m
2
, a range where
creatinine-based formulae for estimating GFR are particularly
inaccurate, either validation of the formula against inulin
clearance in black African populations or validation of the
results of the present study in other populations where obesity
or the associated lipid or glucose abnormalities contribute
little to reductions in eGFR, but where insulin resistance and
adipocytokines may play a role, is required.
Third, we assessed the impact of resistin and CRP alone on
eGFR and failed to evaluate the several additional adipocytokine
changes that may influence eGFR. This was necessary to avoid
the statistical imitations of multiple comparisons that would
have been required if multiple adipocytokines (comparisons with
multiple biomarkers) were evaluated. Consequently, we are likely
to have underestimated the contribution of obesity-associated
inflammatory changes to reductions in eGFR. Notwithstanding
this possibility, we focused on resistin, as of all the adipokines,
resistin demonstrates the most consistent and robust relationships
with renal dysfunction.
16,18-26,28,29
Despite assessing the role of only
one specific adipocytokine, we were able to show a combined
effect of resistin and insulin resistance on eGFR, which was
substantially greater than that of the combined impact of
conventional risk factors, including adiposity indices
per se
.
Nevertheless, the potential role of the multitude of additional
adipocytokines requires further evaluation.
Fourth, we failed to identify CKD from urinary albumin-to-
creatinine ratios in addition to eGFR, thus avoiding the impact
of obesity-associated hyperfiltration on eGFR. However, the
impact of HOMA-IR or resistin concentrations on eGFR was
similar in obese versus non-obese participants.
Last, as the impact of HOMA-IR and resistin on eGFR
were beyond obesity and associated metabolic changes, the
question remains as to the factors responsible for HOMA-IR
and increases in resistin in the community studied. Whether
human immunodeficiency virus infection, the treatment
thereof, or alternative factors contribute therefore requires
further study.
Conclusions
We show in a large community-based sample with a high
prevalence of obesity that the combined impact of insulin
resistance, as indexed by HOMA-IR and circulating resistin
concentrations, on eGFR or CKD was greater than that of all
modifiable conventional cardiovascular risk factors together
(including metabolic syndrome features). Importantly these
effects were beyond even ambulatory or aortic BP and aortic
stiffness. These data suggest that targeting conventional risk
factors alone or the metabolic syndrome
per se
may result
in a marked residual impact on the development of CKD in
communities with a high prevalence of obesity. To adequately
address the public health burden of CKD, approaches may
therefore be required that influence insulin resistance and
the adverse effects of resistin beyond obesity and associated
metabolic syndrome features.
This study would not have been possible without the voluntary collabora-
tion of the participants and the excellent technical assistance of Mthuthuzeli
Kiviet, Nomonde Molebatsi, Delene Nciweni and Nkele Maseko. This work
was supported by the Medical Research Council of South Africa, Circulatory
Disorders Research Trust, University Research Council of the University of
the Witwatersrand, National Research Foundation of South Africa and the
Carnegie Programme.
References
1.
Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU,
et
al
. Chronic kidney disease as a global public health problem: approaches
and initiatives – a position statement from Kidney Disease Improving
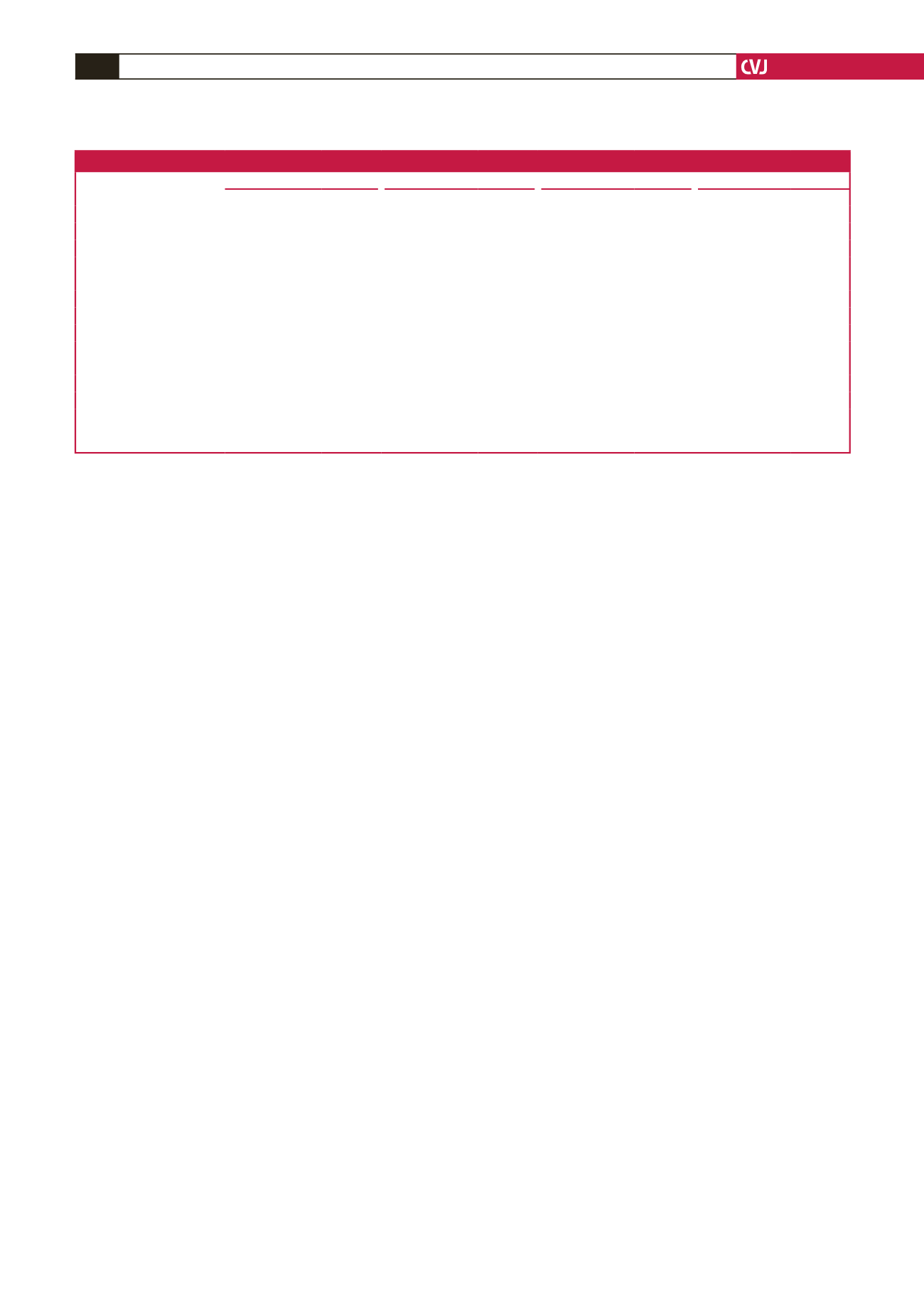
Table 11. Relative impact [standardised slopes (
β
-coefficients)] of factors accounting for chronic kidney disease in a community sample
Models with (n
=
CKD/total)
Brachial SBP (404/984)
24-hour SBP (279/669)
Aortic SBP (400/977)
Aortic PWV (348/876)
CKD versus
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
Age
0.59
±
0.04
<
0.0001
0.57
±
0.04
<
0.0001
0.59
±
0.04
<
0.0001
0.56
±
0.04
<
0.0001
HOMA-IR
0.12
±
0.03
<
0.0001
0.09
±
0.04
<
0.02
0.12
±
0.03
<
0.0001
0.11
±
0.03
<
0.0005
Resistin
0.07
±
0.03
<
0.02
0.08
±
0.03
<
0.02
0.06
±
0.03
<
0.05
0.07
±
0.03
<
0.02
Diabetes mellitus
0.05
±
0.04
0.20
0.02
±
0.04
0.65
0.05
±
0.04
0.20
0.04
±
0.04
0.37
Hypertension
0.02
±
0.04
0.62
–0.03
±
0.04
0.46
0.01
±
0.04
0.76
0.02
±
0.04
0.57
HbA
1c
–0.03
±
0.04
0.50
–0.03
±
0.04
0.54
–0.03
±
0.04
0.47
–0.03
±
0.04
0.48
Waist circumference
–0.06
±
0.04
0.10
–0.02
±
0.04
0.68
–0.07
±
0.04
0.07
–0.06
±
0.04
0.14
Metabolic syndrome
–0.02
±
0.04
0.68
–0.07
±
0.05
0.21
–0.01
±
0.05
0.84
–0.03
±
0.05
0.53
Brachial SBP
0.02
±
0.03
0.56
–
–
–
–
–
–
24-hour SBP
–
–
0.007
±
0.037
0.85
–
–
–
–
Aortic SBP
–
–
–
–
0.005
±
0.036
0.88
–
–
Aortic PWV
–
–
–
–
–
–
0.07
±
0.04
0.06
CKD, chronic kidney disease; SBP, systolic blood pressure; PWV, pulse-wave velocity;
β
-coeff, standardised
β
-coefficient; HOMA-IR, homeostasis model of insulin
resistance. Also included in the regression models were gender, regular tobacco use and regular alcohol consumption. CKD was identified as eGFR values
<
90 ml/
min/1.73 m
2
from eGFR determined using the Chronic Kidney Disease Epidemiology equation.



















