
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 2, March/April 2020
AFRICA
99
blood cells, often originating from inflamed adipose tissue
at a visceral level, indeed supports the notion that inflamed
adipose tissue contributes to the development of kidney injury.
However, clinically, direct measures of visceral fat (computer-
assisted tomography or ultrasound) are not considered to be
conventional risk factors and therefore a large component of the
adverse effects of adiposity on renal function that are mediated
by insulin resistance or resistin will go undetected.
Although relationships between either insulin resistance
or circulating adipocytokine concentrations and eGFR have
been demonstrated on several previous occasions,
12-14,18,21,25,26,28,29,37
these relationships have employed conventional office BP as the
haemodynamic adjustor. In this regard, none of these studies
has considered the possibility that adjustments for conventional
office BP measurements are inadequate for discounting the
haemodynamic actions of insulin resistance, inflammatory
changes or obesity
per se
. In this regard, obesity effects on
BP, which are likely to be induced in part by insulin resistance,
are not detected using office BP measurements alone. Indeed,
obesity results in masked effects on in-office BP.
39
Moreover, both insulin resistance
40
and inflammatory
adipocytokines
41
may cause increases in aortic stiffness,
and through an impact on aortic impedance, may produce
renal microvascular damage beyond brachial BP. Hence, it
is uncertain whether relationships between insulin resistance
or adipocytokines and eGFR
12-14,18,21,25,26,28,29,37
are indeed beyond
the adverse haemodynamic effects of these changes. However,
in the present study, relationships between HOMA-IR or
resistin concentrations and eGFR were largely unaffected by
adjustments for 24-hour BP, aortic BP or aortic PWV. The
present study therefore suggests that the actions of insulin
resistance or resistin are distinct from that of the adverse
haemodynamic consequences of these alterations.
Limitations
There are several limitations to this study. It is cross-sectional
in design and hence the relationships noted may not be
causal, and reverse causality may account for several of the
relationships noted. In this regard, the relationship between
resistin concentrations and eGFR in this study may reflect a
shared genetic background
42
rather than an adverse effect of
resistin on kidney function. However, as demonstrated by us,
the relationships are as robust in unrelated participants (parents
alone) as in related participants (parents and their children and
siblings), suggesting that a shared genetic background is unlikely
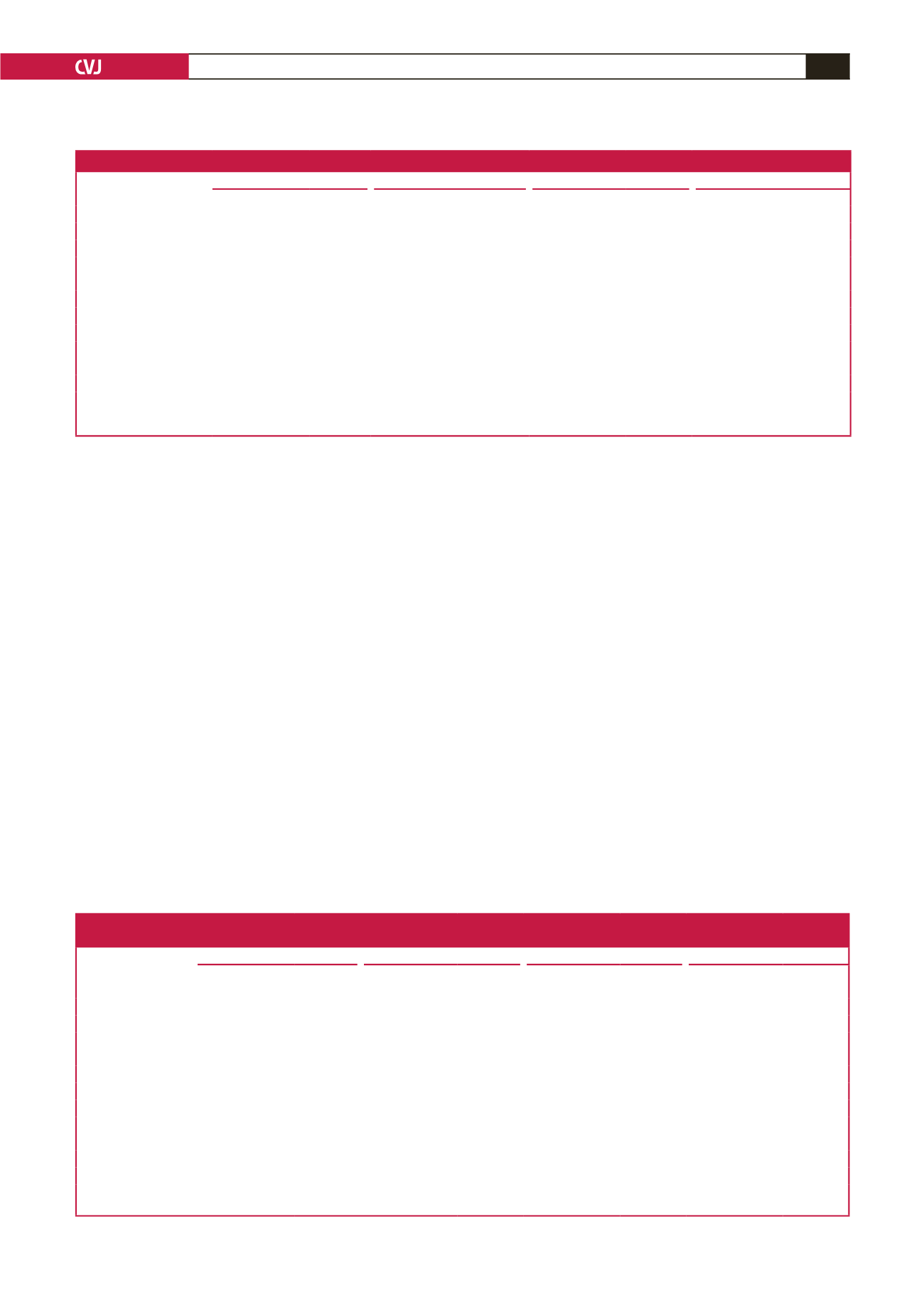
Table 9. Relative impact [standardised slopes (
β
-coefficients)] of factors accounting for CKD in non-diabetic participants of a community sample
Models with (n
=
CKD/total) Brachial SBP (326/850)
24-hour SBP (225/584)
Aortic SBP (322/843)
Aortic PWV (281/762)
CKD versus
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
Age
0.58
±
0.04
<
0.0001
0.56
±
0.05
<
0.0001
0.58
±
0.04
<
0.0001
0.57
±
0.05
<
0.0001
HOMA-IR
0.11
±
0.03
<
0.0005
0.08
±
0.04
<
0.05
0.11
±
0.03
<
0.0005
0.11
±
0.03
<
0.002
Resistin
0.06
±
0.03
<
0.03
0.07
±
0.03
<
0.05
0.07
±
0.03
<
0.02
0.08
±
0.03
<
0.02
Hypertension
0.005
±
0.039
0.90
0.04
±
0.04
0.31
0.01
±
0.04
0.80
–0.01
±
0.04
0.83
Waist circumference
–0.08
±
0.04
<
0.05
–0.04
±
0.05
0.35
–0.09
±
0.04
<
0.03
–0.06
±
0.04
0.15
Glucose
0.04
±
0.03
0.18
0.06
±
0.04
0.13
0.04
±
0.03
0.18
0.05
±
0.04
0.20
Metabolic syndrome
–0.009
±
0.045
0.84
–0.08
±
0.05
0.14
–0.01
±
0.04
0.88
–0.05
±
0.05
0.33
Brachial SBP
–0.01
±
0.04
0.79
–
–
–
–
–
–
24-hour SBP
–
–
0.01
±
0.04
0.72
–
–
–
–
Aortic SBP
–
–
–
–
–0.02
±
0.04
0.63
–
–
Aortic PWV
–
–
–
–
–
–
0.04
±
0.04
0.35
CKD, chronic kidney disease; SBP, systolic blood pressure; PWV, pulse-wave velocity;
β
-coeff, standardised
β
-coefficient; HOMA-IR, homeostasis model of insulin
resistance. Also included in the regression models were gender, regular tobacco use and regular alcohol consumption. CKD was identified as eGFR values
<
90 ml/
min/1.73 m
2
from eGFR determined using the Chronic Kidney Disease Epidemiology equation.
Table 10. Relative impact [standardised slopes (
β
-coefficients)] of factors accounting
for variations in estimated glomerular filtration rate in a community sample
Models with
Brachial SBP (n
=
984)
24-hour SBP (n
=
669)
Aortic SBP (n
=
977)
Aortic PWV (n
=
876)
eGFR versus
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
β
-coeff
±
SEM
p
-value
Age
–0.67
±
0.03
<
0.0001
–0.67
±
0.04
<
0.0001
–0.66
±
0.03
<
0.0001
–0.64
±
0.04
<
0.0001
HOMA-IR
–0.13
±
0.02
<
0.0001
–0.12
±
0.03
<
0.0001
–0.13
±
0.02
<
0.0001
–0.14
±
0.03
<
0.0001
Resistin
–0.12
±
0.02
<
0.0001
–0.12
±
0.03
<
0.0001
–0.12
±
0.02
<
0.0001
–0.12
±
0.02
<
0.0001
Diabetes mellitus
0.005
±
0.030
0.87
0.009
±
0.036
0.80
0.003
±
0.030
0.92
–0.007
±
0.032
0.83
Hypertension
0.02
±
0.03
0.42
–0.02
±
0.04
0.60
0.02
±
0.03
0.49
–0.006
±
0.032
0.84
HbA
1c
0.009
±
0.031
0.77
–0.005
±
0.038
0.89
0.009
±
0.031
0.78
0.031
±
0.033
0.34
Waist circumference
0.05
±
0.03
0.08
0.05
±
0.04
0.18
0.06
±
0.03
0.07
0.04
±
0.03
0.27
Metabolic syndrome
–0.003
±
0.037
0.93
0.005
±
0.044
0.90
–0.008
±
0.037
0.84
0.015
±
0.039
0.71
Brachial SBP
–0.09
±
0.03
<
0.005
–
–
–
–
–
–
24-hour SBP
–
–
–0.04
±
0.03
0.21
–
–
–
–
Aortic SBP
–
–
–
–
–0.08
±
0.03
<
0.01
–
–
Aortic PWV
–
–
–
–
–
–
–0.09
±
0.03
<
0.005
eGFR, estimated glomerular filtration rate; SBP, systolic blood pressure; PWV, pulse-wave velocity;
β
-coeff, standardised
β
-coefficient; HOMA-IR, homeostasis model
of insulin resistance. Also included in the regression models were gender, regular tobacco use and regular alcohol consumption.



















