CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 1, February 2012
e12
AFRICA
Due to the lack of pulses in the bilateral upper extremities,
aortography was performed. The image of a thrombus extending
from the brachiocephalic trunk to the right subclavian artery and
the right common carotid artery was seen. Thrombus was also
present in the left axillary artery (Fig. 2A, B).
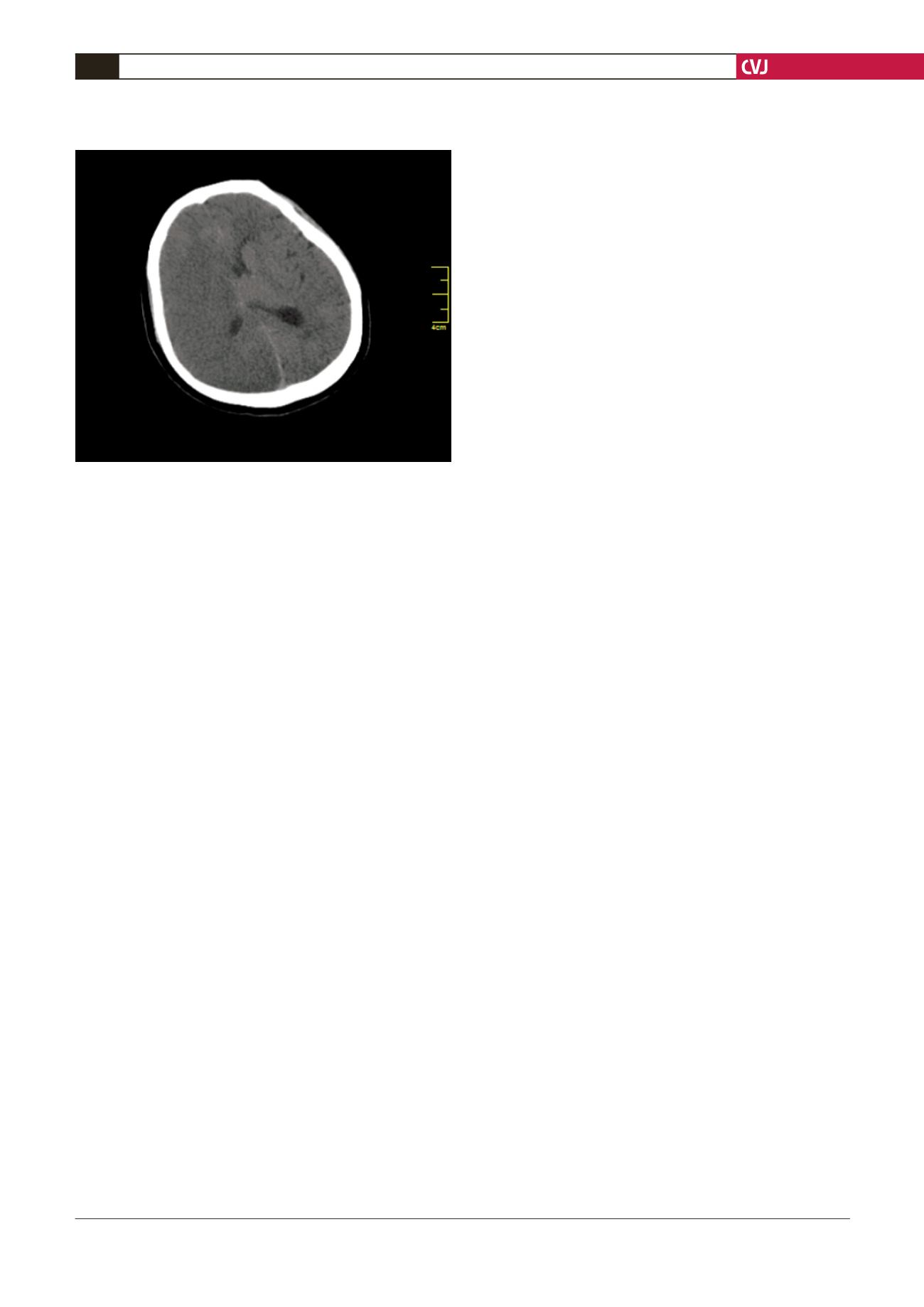
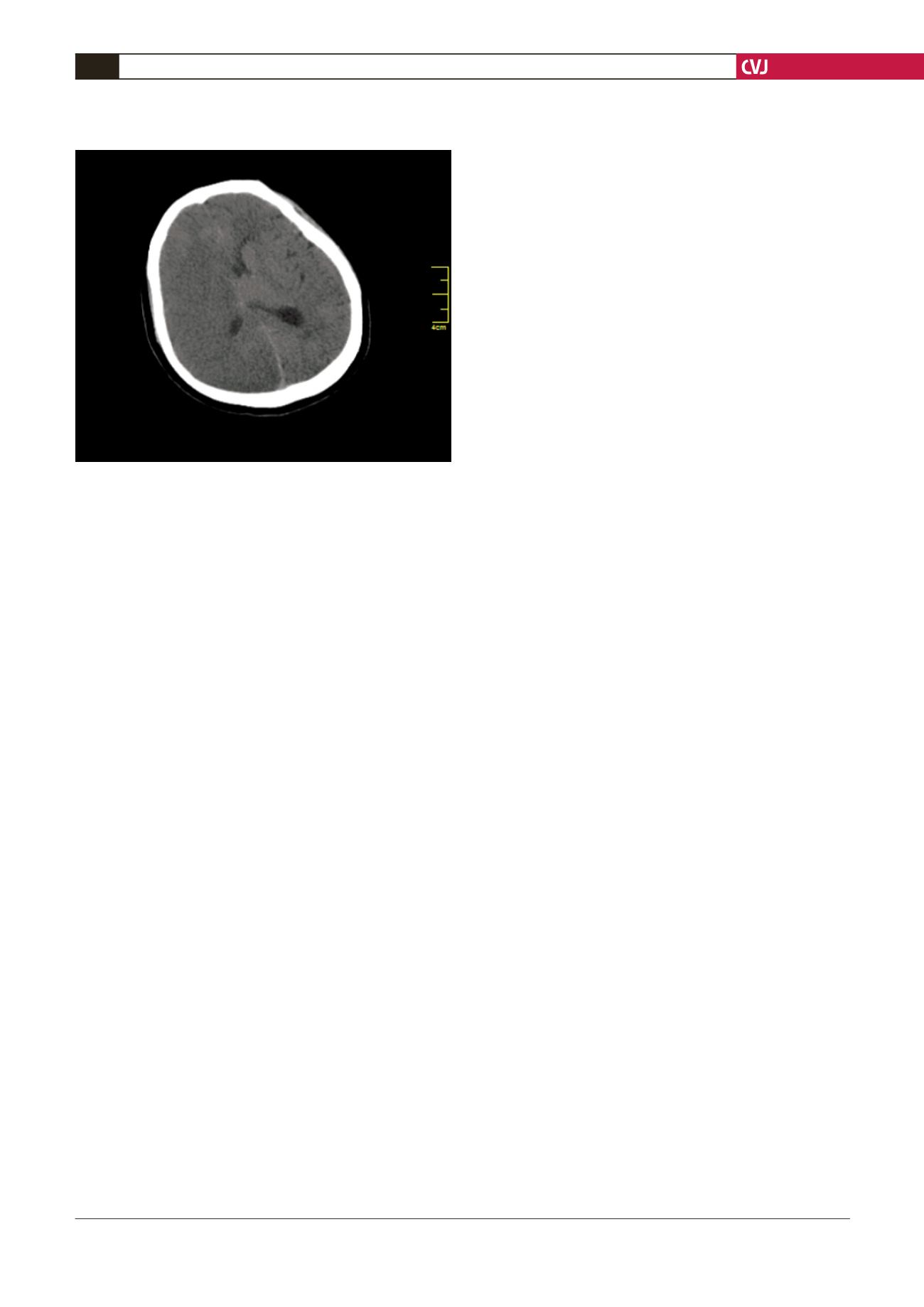
Neurologically, the Glasgow coma scale of 3 was established.
On computed tomography, we identified massive oedema and
hypodense areas on the right cerebral hemisphere, indicating
infarction (Fig. 3). As thrombolytic treatment was being planned,
he had a cardiac arrest. The patient did not respond to resuscita-
tion and died.
Discussion
In the follow up of repaired TOF patients, it is common to
see complications such as residual ventricular septal defect
(10–20%), aortic insufficiency, pulmonary stenosis and pulmo-
nary regurgitation. Such conditions may sometimes require a
further operation.
4
The most important difficulty, however, is the
risk of SCD. In a multicentre study of 793 patients carried out
by Gatzoulis
et al
., 10.4% developed atrial flutter/fibrillation,
11.9% experienced sustained ventricular tachycardia and 8.3%
died suddenly 35 years after the operation.
In this study, middle age, pulmonary regurgitation and a
QRS duration
>
180 ms were identified as the key risk factors.
3
Several studies propose a variety of risk factors for SCD, includ-
ing prior palliative shunt, inducible sustained ventricular tachy-
cardia, QRS
>
180 ms, ventriculotomy incision, non-sustained
ventricular tachycardia and left ventricular end-diastolic pressure
>
12 mmHg.
5
Other studies have emphasised that pulmonary
regurgitation, right ventricular dilatation and previous palliative
shunt carry a higher risk for SCD.
5
In a study by Harrison
et al
., the development of atrial tach-
yarrhythmia (AT) was found to be associated with substantial
mortality, including ventricular tachycardia, stroke and death
[combined events, 20 of 29 patients (69%)]. The development of
AT in the adult long after TOF repair identifies patients at risk
and is associated with older age at repair, a higher frequency of
haemodynamic abnormalities and increased morbidity.
6
Given these risk factors, our patient was in the moderate-risk
group with respect to arrhythmia. It has been suggested that
preventive measures for SCD, including implantable cardiovert-
er-defibrillator (ICD), are necessary in patients at high risk.
7
Our patient experienced palpitations, possibly due to atrial or
ventricular arrhythmia, for one week before the embolism. As
he was brought in after 30 minutes of resuscitation and during
which cardioversion was performed twice, the differentiation of
arrhythmia could not be done. However, it is known that intra-
cardiac thrombus has been found after 48-hour, or even shorter
duration of stasis and stunning in various transoesophageal
echocardiography studies.
8-10
Furthermore, in the blood sample
taken from the patient on the day of the incident, no mutation
was observed other than prothrombin G20210A heterozygote
mutation, which has only a weak relation to thrombosis.
11
Conclusion
We report this striking case of massive embolism leading to
cardiac arrest in a patient 30 years after a TOF operation and
consider whether the cause could have been an intracardiac
thrombus and systemic embolism secondary to arrhythmia.
References
1.
Yap SC, Haris L. Sudden cardiac death in adults with congenital heart
desease.
Expert Rev Cardiovasc Ther
2009;
7
(12): 1605–1620.
2.
Murphy JG, Gersh BJ, Mair DD,
et al
. Long-term outcome in patients
undergoing surgical repair of tetralogy fallot.
N Engl J Med
1993;
329
:
593–599.
3.
Gatzoulis MA, Balaji S, Webber SA,
et al
. Risk factors for arrhythmia
and sudden cardiac death late after repair of tetralogy of fallot: a multi-
center study.
Lancet
2000;
356
: 975–981.
4.
Brıckner ME, Hillis LD, Lange RA. Congenital heart desease in adults.
Second of two parts.
N Engl J Med
2000;
342
: 334–342.
5.
Khairy P, Dore A, Poirier N,
et al
. Risk stratification in surgically
repaired tetralogy of fallot.
Expert Rev. Cardiovasc Ther
2009;
7
:
755–762.
6.
Harrison DA, Siu SC, Hussain F, MacLoghlin CJ, Webb GD, Harris L.
Sustained atrial arrhythmias in adults late after repair of tetralogy of
Fallot.
Am J Cardiol
2001;
87
(5): 584–588.
7.
Monro JL. Late outcomes following repair of fallot.
Eur J Cardiothorac
Surg
2009;
35
: 165–166.
8.
Stoddard MF, Dawkins PR, Prince CR,
et al
. Left atrial appendage
thrombus is not uncommon in patients with acute atrial fibrillation and
a recent embolic event: a transesophageal echocardiographic study.
J
Am Coll Cardiol
1995;
25
: 452–459.
9.
Manning WJ, Silverman DI, Waksmonski CA,
et al
. Prevalence of
residual left atrial thrombi among patients with acute thromboembo-
lism and newly recognized atrial fibrillation.
Arch Intern Med
1995;
13
: 2193–2198.
10. ACC/AHA/ESC 2006 Guidelines for the management of patients with
atrial fibrillation.
J Am Coll Cardiol
2006;
48
: 149–246.
11. Martinelli I, Battaglioli T, Bucciarelli P,
et al
. Risk factors and recur-
rence rate of primary deep vein thrombosis of the upper extremities
Circulation
2004;
110
: 566–570.
Fig. 3. Massive oedema on the right cerebral hemisphere
and hypodense areas on the CT scan.