
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
AFRICA
271
device) could contribute towards more
effective management of STEMI in South
Africa. In addition, the societal cost of
an undertreated STEMI population will
be estimated to determine the potential
financial impact of the intervention as
well the cost benefits of the treatment
modalities (PCI and fibrinolysis).
International collaboration has been
established between the South African
Society of Cardiovascular Intervention
(SASCI), STEMI India (who developed
the software and the model) and Stent-
for-Life (SFL) Europe to pursue these
objectives. SAHA applied for membership
as affiliated country of SFL Europe, an
initiative of the European Association
of Percutaneous Cardiovascular Inter-
ventions (EAPCI) and Prof Rhena
Delport (regional editor for South Africa
of the
Cardiovascular Journal of Africa
and project manager for SFL South
Africa) signed the declaration of intent,
on behalf of SASCI, on 27 February 2016,
to fulfil the SFL mission in South Africa.
SAHA has thus positioned itself in the
frontline of STEMI care and hopefully,
with concerted action among all role
players in STEMI management in South
Africa, STEMI outcomes will improve and
the cardiovascular disease-related burden
of disease will be managed appropriately.
Rhena Delport
1.
Kengne AP, Mayosi BM. Readiness of the
primary care system for non-communicable
diseases in sub-Saharan Africa.
Lancet Glob
Health
2014;
2
(5): e247–248.
2.
Hertz JT, Reardon JM, Rodrigues CG, de
Andrade L, Limkakeng AT, Bloomfield GS,
Lynch CA. Acute myocardial infarction in
sub-Saharan Africa: the need for data
. PLoS
One
2014;
9
(5): e96688.
3.
Use of health facilities and levels of
selected health conditions in South Africa:
Findings from the General Household
Survey, 2011. Statistics South Africa.
Report no. 03-00-05 (2011).http://www.
statssa.gov.za/publications/Report-03-00-05/Report-03-00-052011.pdf.
4.
Meel R, Gonçalves R. Time to fibrinolytics
for acute myocardial infarction: Reasons for
delays at Steve Biko Academic Hospital,
Pretoria, South Africa
. S Afr Med J
2015;
106
(1): 92–96.
5.
Maharaj RC, Geduld H, Wallis LA. Door-
to-needle time for administration of fibrino-
lytics in acute myocardial infarction in Cape
Town.
S Afr Med J
2012;
102
(4): 241–244.
6.
Schamroth C; ACCESS South Africa inves-
tigators. Management of acute coronary
syndrome in South Africa: insights from
the ACCESS (Acute Coronary Events – a
multinational survey of current management
strategies) registry.
Cardiovasc J Afr
2012;
7
:
365–370.
7.
Snyders A, Delport R. The SA Heart
STEMI Early Intervention Project. Referral
pathways for reperfusion of STEMI – devel-
oping strategies for appropriate intervention
.
SA Heart J
2015;
12
: 72–80.
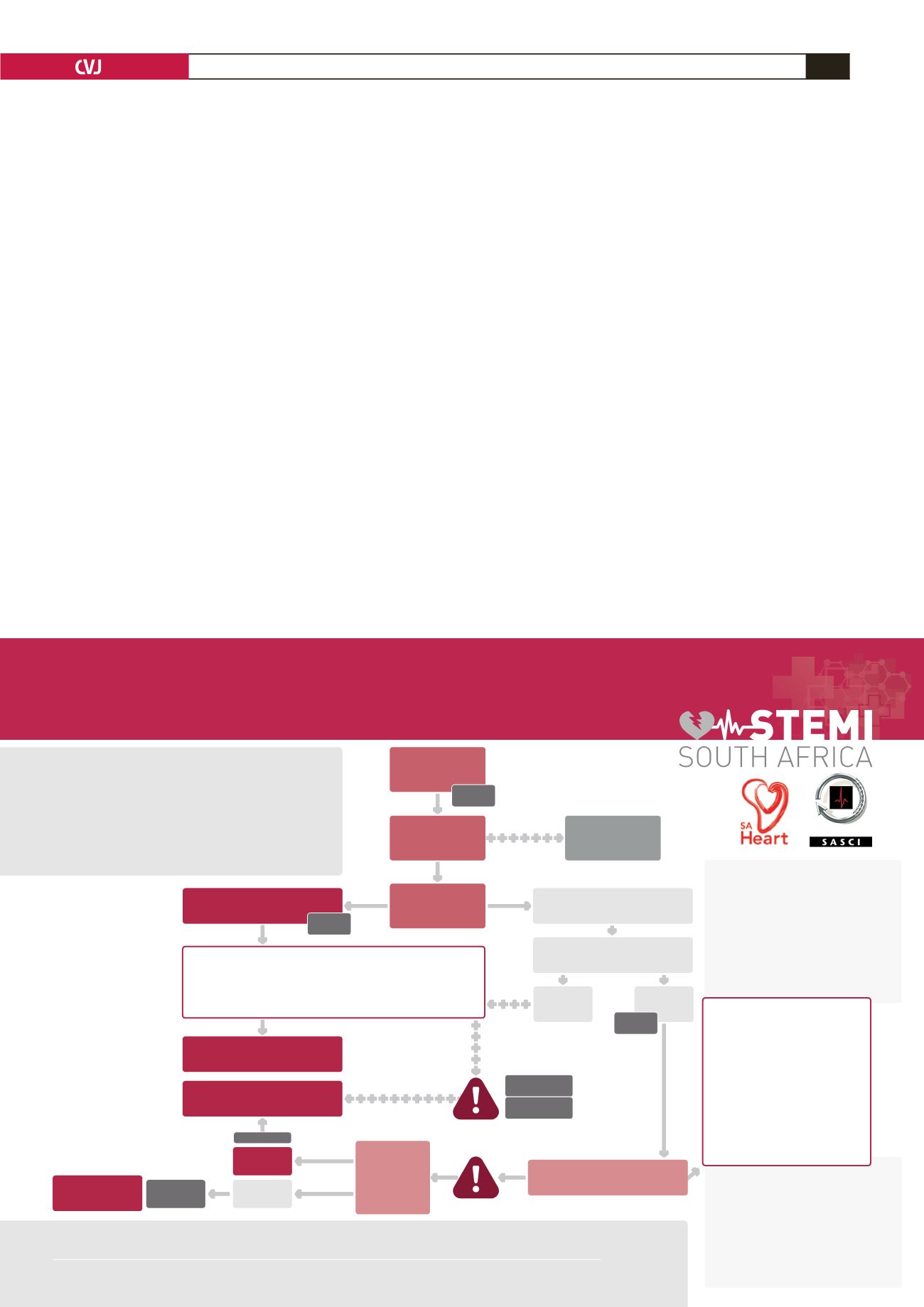
Thrombolysis RELATIVE Contra-indications
• Transient ischaemic attack in the preceding
6 months
• Oral anticoagulant therapy
• Pregnancy or within 1 week postpartum
• Refractory hypertension
(systolic blood pressure > 180 mmHg and/or
diastolic blood pressure > 110 mmHg)
• Advanced liver disease
• Infective endocarditis
• Active peptic ulcer
• Prolonged or traumatic resuscitation
Thrombolysis ABSOLUTE Contra-indications
• Previous intracranial haemorrhage or stroke of
unknown origin at any time
• Ischaemic stroke in the preceding 6 months
• Central nervous system damage or neoplasms
or atrioventricular malformation
• Recent major trauma/surgery/head injury
(within the preceding 3 weeks)
• Gastrointestinal bleeding within the past month
• Known bleeding disorder (excluding menses)
• Aortic dissection
• Non-compressible punctures in the past 24 h
(e.g. liver biopsy, lumbar puncture)
MEDICATION
to administer with fibrinolytic therapy
• Tenecteplase
(TNK–tPA)
Single i.v. bolus:
30 mg if < 60 kg
35 mg if 60 to < 70 kg
40 mg if 70 to < 80 kg
45 mg if 80 to < 90 kg
50 mg if ≥ 90 kg
• Streptokinase
(SK)
1.5 million units over
30 – 60 min i.v.
• Loading dose Aspirin 150-500 mg
orally or 250 mg IV
• Loading dose Clopidogrel 300 mg
orally if aged ≤ 75 years
ECG = electrocardiogram
FMC = first medical contact
STEMI = ST-segment elevation myocardial
infarction
PCI
= Percutaneous coronary intervention
Monitor every
10 min if chest
pain persists
Immediate
Fibrinolysis
EMS or non-primary-PCI
capable centre
YES
NO
Preferably
< 60 min
Immediate
transfer to
PCI center
Primary-PCI
capable centre
MEDICATION
to administer before primary PCI
•
Loading dose Aspirin 150 - 300 mg orally or 80 - 150 mg IV
•
Loading dose Clopidogrel 600 mg orally if aged ≤ 75 years
OR
Loading dose Prasugrel 600 mg orally
Patient has
chest pain
Diagnosis with
12 lead ECG
STEMI
diagnosis*
Preferably
< 10 min
YES
NO
PCI possible in
< 120 min?
Preferably
3 - 24
hours
Primary-PCI
Rescue PCI
Coronary
Angiography
Successful
Fibrinolysis?
Immediately
Immediate transfer
to PCI center
Preferably
< 90 min
≤ 60 min for
early presenters
Preferably
< 30 min
Dr Adriaan Snyders
- National Champion for project 082 446 1558
Prof Rhena Delport
- Project Manager 082 445 4500
CONTACT INFORMATION:
Reference: 1.
ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012 Oct;33(20):2569-619.
doi: 10.1093/eurheartj/ehs215.
2.
http://www.heartfoundation.co.za/how-your-heart-works/symptoms-heart-attack(accessed on 7 Feb 2013)
SA Heart Association Early Reperfusion Project
TIME TO
REPERFUSION
IS CRITICAL

















